Anthrax is a severe infectious disease caused by the bacterium Bacillus anthracis. It is a zoonotic disease, meaning it primarily affects animals, particularly herbivores such as cattle, sheep, goats, and horses. However, humans can also contract anthrax through exposure to infected animals or animal products.
Anthrax: Types and Transmission
Anthrax infection can occur in four main forms, each with a distinct mode of transmission:
- Cutaneous Anthrax: This is the most common form of anthrax, accounting for about 95% of cases. It occurs when spores of B. anthracis enter the body through a cut or abrasion in the skin, typically after handling infected animals or animal products (such as wool, hides, or hair).
- Inhalation Anthrax: Also known as Woolsorter’s disease, this form results from inhaling anthrax spores, usually in occupational settings where animal products are processed (e.g., textile mills).
- Gastrointestinal Anthrax: This rare form is caused by consuming contaminated meat from an infected animal that hasn’t been cooked thoroughly.
- Injection Anthrax: A rare form primarily seen in people who inject drugs. It results from injecting contaminated drugs.
Anthrax Symptoms: Recognizing the Signs
The symptoms of anthrax vary depending on the type of infection:
1. Cutaneous Anthrax:
- Starts as a painless, itchy bump that resembles an insect bite.
- Develops into a small blister, then a painless ulcer with a black center (eschar) within 1-2 days.
- Swelling may occur around the ulcer.
2. Inhalation Anthrax:
- Initial symptoms resemble a common cold (fever, cough, chest discomfort, muscle aches).
- Progresses rapidly to severe breathing problems, fever, and shock.
3. Gastrointestinal Anthrax:
- Symptoms include fever, nausea, vomiting, abdominal pain, bloody diarrhea.
- Can lead to severe complications such as sepsis and shock.
4. Injection Anthrax:
- Symptoms similar to cutaneous anthrax but can spread more rapidly throughout the body.
- Fever, chills, and abscesses at the injection site.
Anthrax Prevention: Protecting Yourself and Your Community
Anthrax prevention strategies vary depending on the risk factors involved:
- Vaccination: An anthrax vaccine is available for high-risk individuals, such as military personnel, laboratory workers, and certain livestock handlers.
- Animal Vaccination: Vaccinating livestock in anthrax-endemic areas can reduce the risk of infection in both animals and humans.
- Proper Handling of Animal Products: People who work with animal hides, wool, or hair should wear protective clothing (gloves, masks) to prevent exposure to spores.
- Safe Food Preparation: Ensure meat is thoroughly cooked to kill any potential anthrax spores.
MedicW: Medical Consumables in Anthrax Prevention and Management
- Protective Apparel: MedicW provides a comprehensive range of PPE, including disposable gloves, gowns, masks, and eye protection, vital for preventing exposure to anthrax spores in both healthcare and industrial settings.
- Sampling Swabs: MedicW’s sterile swabs are essential for collecting samples from suspected anthrax lesions for laboratory testing and confirmation of the diagnosis.
- Respiratory Protection: High-quality N95 respirators, offered by MedicW, are crucial for protecting healthcare workers and first responders from inhaling anthrax spores in the event of an outbreak or during patient care.
- Biohazard Bags: MedicW’s biohazard bags provide safe and secure disposal of contaminated materials, minimizing the risk of spreading anthrax spores.
Anthrax Treatment
Anthrax is treated with antibiotics, such as ciprofloxacin, doxycycline, or penicillin. The type of antibiotic and the length of treatment depend on the type of anthrax infection and the individual’s medical history. Early diagnosis and treatment are essential for a favorable outcome.
Anthrax FAQs: Your Questions Answered
1. Is Anthrax contagious?
Answer: Anthrax is not highly contagious from person to person. Cutaneous anthrax is rarely, if ever, spread from person to person. Inhalation anthrax, although not easily transmitted, could potentially spread through close contact with a patient who is actively coughing or sneezing.
2. What should I do if I think I’ve been exposed to Anthrax?
Answer: Seek medical attention immediately. If you’ve had a possible exposure to anthrax spores, your doctor may prescribe antibiotics to prevent infection or treat an existing infection.
3. How is Anthrax diagnosed?
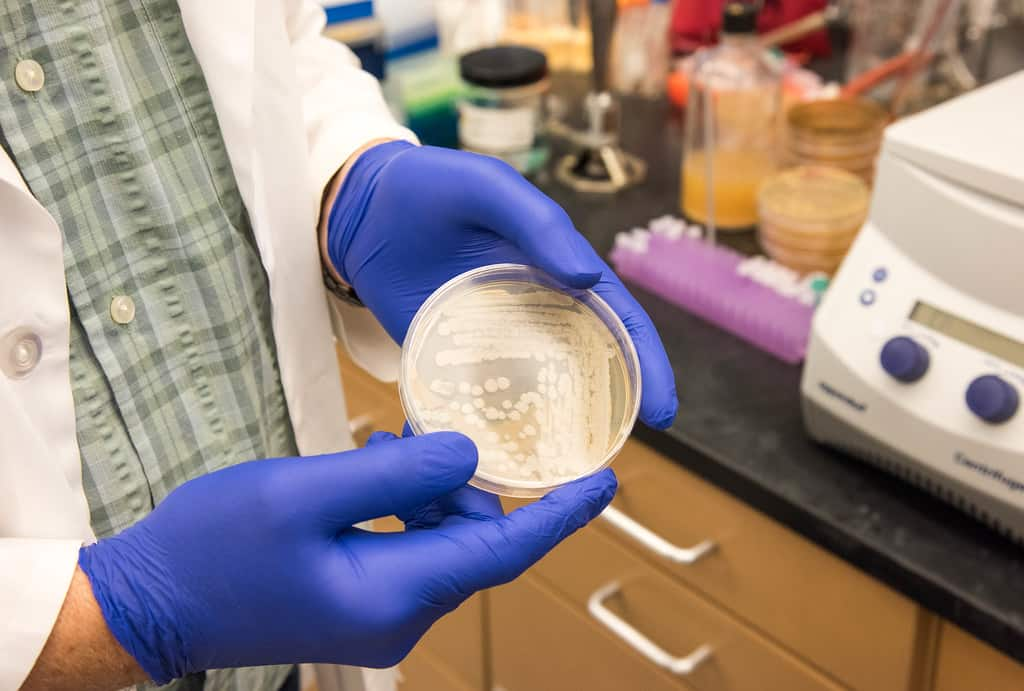
Answer: Anthrax is diagnosed through a combination of physical examination, medical history (including potential exposure), and laboratory tests. Tests may involve examining skin lesions, blood cultures, or samples from the respiratory tract.
4. Is there a vaccine for Anthrax?
Answer: Yes, there is an anthrax vaccine available. However, it’s typically only recommended for people at high risk of exposure, such as military personnel, laboratory workers, or those who handle potentially contaminated animal products.
5. What are the chances of surviving Anthrax?
Answer: The chances of surviving Anthrax depend on the type of infection and how quickly treatment is started. Cutaneous anthrax has a high survival rate if treated promptly. Inhalation anthrax is more serious, with a lower survival rate, even with treatment.
6. Can Anthrax be used as a bioweapon?
Answer: Sadly, anthrax has been weaponized in the past due to the ability of its spores to survive for long periods and their potential to cause severe illness when inhaled. However, significant security measures are in place to prevent and respond to potential bioterrorist threats involving anthrax.
Anthrax: Conclusion
Anthrax, while not a common infection, remains a significant public health concern. By understanding its transmission, recognizing the symptoms, and practicing preventive measures, we can minimize the risk of infection. MedicW’s commitment to providing quality medical supplies empowers healthcare providers, laboratories, and individuals in effectively preventing and managing anthrax outbreaks, ensuring a safer and healthier world.
We emphasize:
- Be aware of anthrax and its potential risks.
- Consult your doctor promptly if you suspect exposure or infection.
- Follow public health advisories related to potential outbreaks.
Together, through vigilance and informed action, we can minimize the threat of anthrax and protect public health.
MedicW is committed to being your trusted partner in providing high-quality medical consumables. Explore our comprehensive range of products and discover how we can support your healthcare needs. Visit us at medicw.com or contact our team at [email protected].
Link to this article: Anthrax: Understanding, Preventing, and Managing the Threat
